This interview with Anatomy Trains author Tom Myers first appeared in the Huffington Post.
What is the most plentiful tissue in the body — and the most ignored?
The answer is fascia — the gooey, gliding stuff that holds you together. Fascia is a broad term for the extracellular matrix of fibers, “glue” and water surrounding all your cells, and wrapping like plastic wrap around muscle fibers and muscles, organs, bones, blood vessels and nerves — and finally as a second skin around your entire body.
“Fascia is like the Cinderella tissues of the body,” says Tom Myers, a leading thinker in integrative anatomy and author of Anatomy Trains. “It has been the most ignored of all the tissues in the body — at least up until recently. Yet, fascia is critical to understanding the body and what it takes to keep your body functional and healthy all life long.”
In recent years, the interest in fascia has surged. In 2007, fascial researchers and practitioners banded together to initiate the biennial Fascia Research Congress, where researchers and health practitioners can share new discoveries.
Understanding the elusive Cinderella tissues offers an important glimpse into important, yet not widely known, aspects of bodily health and function. Here are four fascinating facts about fascia:
1. All You Learned About “Muscles” Is Wrong
A primary lesson emerging from new research into fascia is that all we learned about muscles is wrong.
“That illustration in your doctor’s office of the red-muscled human body is a body with its fascia cut away,” says Myers. “It’s not what you look like inside, but it’s a lot neater and easier to study. And, it’s the way doctors have been taught to look at you.”
We commonly speak about the musculoskeletal system, and the muscles attached to the bones of the body. But according to Myers, muscles in fact don’t attach to bones. Fascia does.
“Muscle is like hamburger; it can’t attach to a bone,” says Myers. “There’s fascia going around and through the muscle. And when the muscle runs out, that fascia from the outside and the middle of the muscle spins into a tendon, just like yarn.”
It may be useful for our thinking mind to dissect the body in to some 600 muscles and their tendon attachments to bones. However, the body doesn’t think in terms of 600 individual muscles.
“Your brain does not think in terms of biceps and deltoids,” says Myers. “There is one muscle that exists in 600 fascial pockets. Ultimately, the brain creates movement in terms of large fascial networks and individual motor units, not our named muscles.”
2. Much More Than a Wrapping Material
Fascia is not just a passive wrapping material, but a live, biological fabric, which directs the traffic of forces around the body, and responds and remodels itself as forces change.
Some researchers, like Helene Langevin of the University of Vermont, suggest that the connective tissue network may function as a whole-body communications system, which influences the function of all other physiological systems.
How exactly such a whole-body network would be communicating within itself is as yet unknown, and there may be several pathways. Langevin has developed evidence, for example, that the fascial network may correspond to the network of acupuncture points and meridians. In this framework, acupuncture needles produce cellular changes that propagate along connective tissue planes.
A similar effect is created by the stretching of the connective tissue created by yoga poses or externally applied stretch and pressure during bodywork and massage.
3. Redefining Chronic Pain
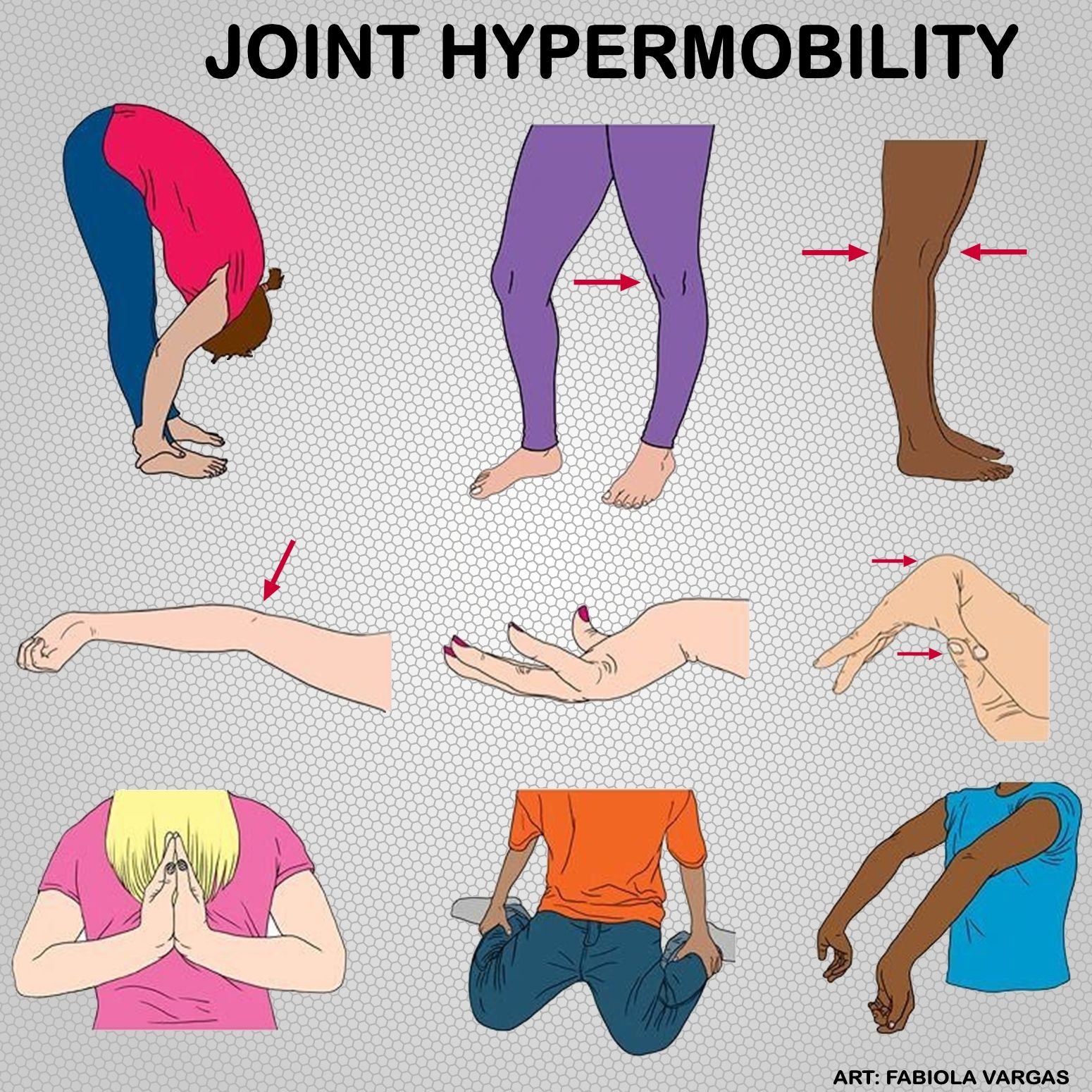
In its healthy state, the fascial network stretches and moves without restriction. However, age, injuries, repetitive stress, poor postural habits and even emotional trauma can cause fascia to lose its flexibility and become tight and restricted.
This helps stabilize the body in the short term, but unfortunately, it also locks you into a chronic strain pattern that can be hard to correct. Think of it like wearing a thin silk suit. If you pull on one part of the suit, the tension patterns will show up throughout.
Fascial strain patterns translate through the entire body, and affect the structural network of the entire body. They may lie at the root of chronic pain issues like migraine headaches, chronic back pain, or fibromyalgia, or other pesky pain problems that just won’t go away.
For this reason, bodywork techniques focusing directly on the fascia, such as Rolfing and myofasical release therapy, can sometimes stimulate tremendous physical and/or emotional release where other modalities come up short.
4. A New Understanding of Fitness
While we usually think in terms of fitness as strong muscles and cardiovascular endurance, we ignore fascia at our own peril. Having an integrated and well-trained fascial network is important not just for anyone engaged in sports, but for anyone wishing to retain a healthy and functional body throughout life.
When you train the body, the fascia is trained as well. However, it may not be the way you would want to train it. If your fitness routine involves mainly machines, you will not end up with a fascial network that is as strong, versatile and capable as you’d like, but rather a one-dimensional network that may respond less efficiently to challenges.
“Exercise machines are great for building individual muscles and terrible for training your fascia, because they train the fascia in one particular direction, one particular vector,” says Myers. “You end up training fascia, which is not prepared for life, because life doesn’t come at you right straight down the same vectors that the machines do.”
In terms of training, Myers says, favour movement forms that involve a lot of variety in direction and load, which builds versatile balance and stability into your body. Yoga asanas are particularly useful for stretching the long chains of fasica in numerous directions ways, offering the kind of system-wide engagement it needs. Training too hard or repeating the same routine without variation can lead to fascial adhesions or injury.